10 minute read
A Brief History
The field of palliative care grew out of the hospice movement in Great Britain in the late 1940s. As the world of medicine was advancing, hospitals were the place one would go to receive end-of-life care. However, not everyone wanted to be in a hospital. If patients knew they were going to be dying within days, why couldn’t they be at home?
This growing movement soon made its way to the United States. It continued to be found that patients were not only living longer, but that patient’s quality of life during that time improved. It is this idea that is at the center of what palliative care is: an approach that improves the quality of life of patients and their families facing the problems associated with a life-limiting condition.
Advances in palliative care and notable research outcomes have since inspired an increase in hospital-based palliative care programs—making symptom management, identification and support of caregiver needs, and coordination of care, more mainstream practices.

Common Misconceptions
Today, when you hear the words “palliative care”, there are likely some questions and misconceptions that arise: What is the difference between palliative care and hospice care? Does receiving palliative care mean I’ll ultimately be receiving hospice care? Or, palliative care isn’t for my loved one if it isn’t pain management we’re seeking; just to name a few. We turned to Nurse Practitioner and 40-year veteran of the palliative care field, Barb Opperwall, to answer these questions and clarify the most common misconceptions.
Misconception #1: Palliative Care and Hospice Care Are the Same
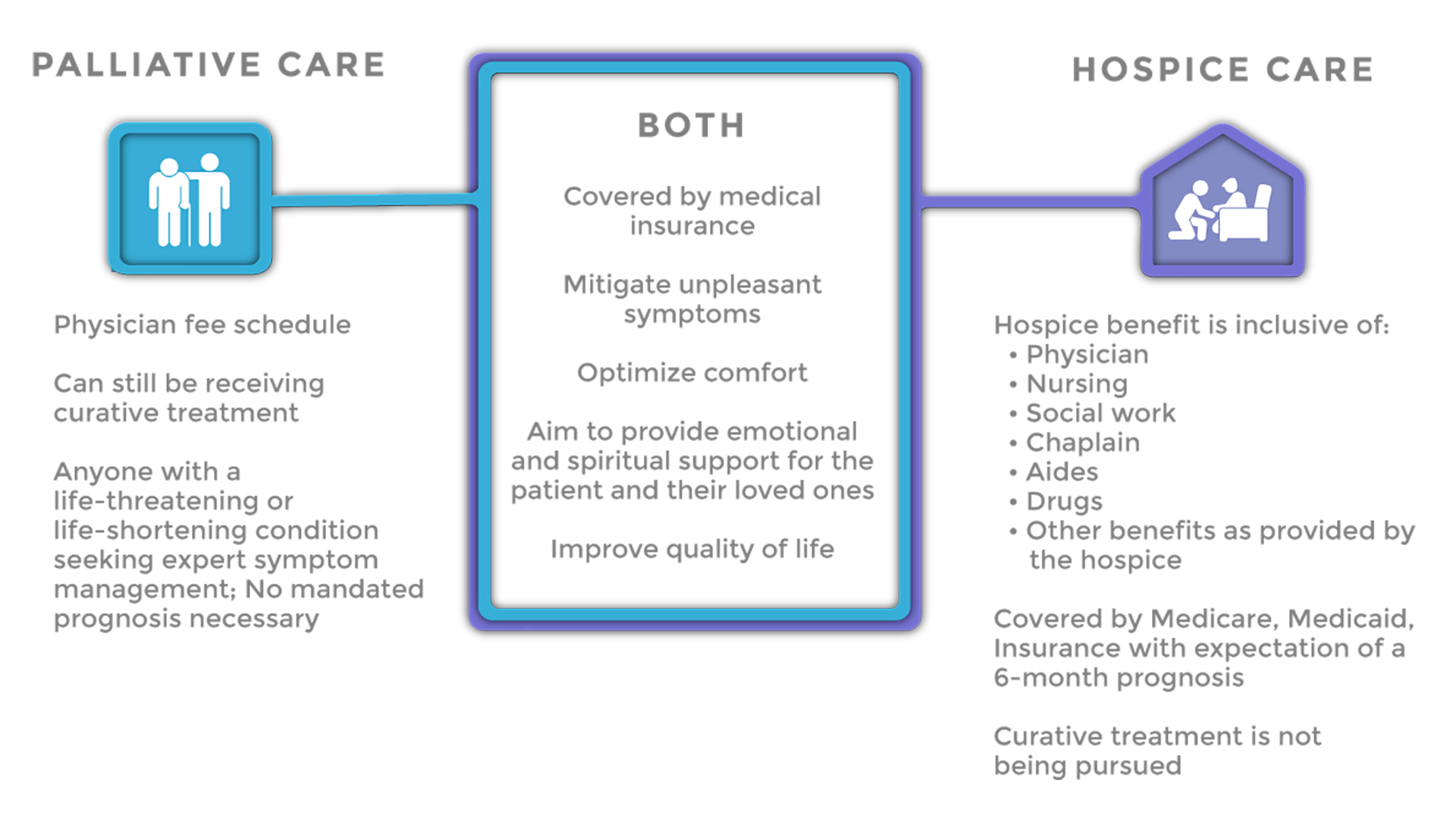
The most common misconception is perhaps that palliative care and hospice care are synonymous with one another. Knowing palliative care emerged out of the hospice care movement, as well as the fact that they share common goals, it’s understandable why one would think that. Although it is an important part of end-of-life care, palliative care is not limited to patients at the end of life. Barb helped to put it simply, noting, “All hospice care is palliative care, but not all palliative care is hospice care.”
A key difference is in the fact that palliative care does not carry the same government-mandated 6-month prognosis that hospice care does; it is for anyone with a life-limiting diagnosis who would benefit from assistance with expert symptom management, patient centered decision making and quality of life concerns.
Non-hospice palliative care recipients can also still be receiving curative treatment for their illness, and can start receiving palliative care as early as the time of their diagnosis. Hospice care recipients are no longer receiving curative treatments however, still use the symptom management and emotional and spiritual support palliative care provides through their end of life.
Misconception #2: Palliative Care is a Pipeline to Hospice
Knowing the types of diagnosis palliative care is associated with, many tend to assume that palliative care is a pipeline to hospice. “Palliative care is really for anyone that has a life-limiting prognosis that is in need of expert symptom management. They are often not separated and people worry palliative care is simply ‘stealth hospice’,” Opperwall explained. “A patient with a cancer diagnosis undergoing chemotherapy and receiving palliative care to manage their chemo symptoms for example, can ‘graduate’ from their palliative care regimen should the cancer be put in remission. And we hope they do.”
Misconception #3: Palliative Care is Pain Management
Barb went on to explain that many also most commonly associate the symptom management piece of palliative medicine with pain management; that people think patients are essentially living in an opioid-induced haze. When in reality, symptom management extends well beyond pain management including everything from digestive symptoms and trouble sleeping to anxiety and itching. Although palliative care uses opiates for pain, it is also adding interventional care and adding more options for pain management.
Misconception #4: The Same Insurance Benefits Apply for Both Palliative Care & Hospice Care
It’s often thought that you can go on palliative care and have the same insurance benefits that cover hospice care. This simply just isn’t true. Most benefit plans limit hospice services to patients with less than six months to live and who are willing to forego further curative treatment. With costs of treatment for those with a longer prognosis being so high, reimbursers have, for a long time, not endorsed it. In fact, Medicare is just starting to explore in-home palliative care; however, private-pay insurance companies still balk at it. Services such as the in-home, around-the-clock care often associated with hospice care are not covered for palliative care recipients.
What Does a Palliative Care Team Do?
One question that arises, then, is how a palliative care team differs from a traditional medical caregiving team. With the number of medications, treatments, and therapies a patient may be taking for a life-limiting condition, Opperwall explains, “Often, symptom management gets erratic. Having a palliative care team with interdisciplinary skills and expertise to manage all of it can be helpful.”
The palliative care team can include a number of different individuals whose roles extend beyond just symptom management. Individuals such as, the patient’s loved ones or others specifically noted in the patient’s Advance Care Plan; a palliative doctor, the patient’s other doctors, and nurses. This team helps to coordinate expert care, helps to navigate the often confusing healthcare system, and provide the emotional support often not addressed by standard medical care. Finally, a palliative care team can also help guide patients in Advance Care Planning.
The Same Goal
Although knowing the differences between palliative care and hospice care is important, ultimately, they work together. As Barb Opperwall concluded plainly, “In the end the goal is the same: to live as long as you can and feel as good as you can while living.”

